Breakthrough therapies - an end to progressive disability? Episode 88
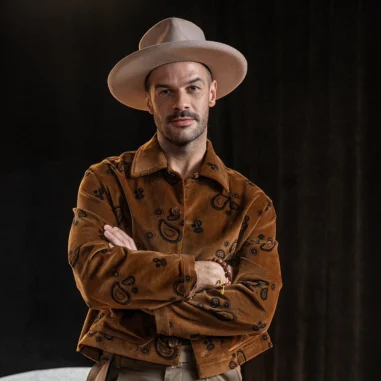
Multiple sclerosis has until recently been associated with irreversible disability, but advances in medicine are opening up new possibilities for patients. In the latest episode of Patient First, Monika Rachtan talks to Dr Elżbieta Jasińska, M.D., about the contemporary approach to MS diagnosis and treatment, discussing how early, high-impact therapy can give patients the chance to live a life free of relapses and progressive disability?
What is multiple sclerosis and how do you recognise it?
Multiple sclerosis (MS) is a chronic autoimmune disease that attacks the central nervous system, in which the myelin sheaths of neurons are damaged [1]. The condition is most commonly diagnosed in young adults aged 20-40 years and can range from mild symptoms that do not significantly affect daily functioning to advanced stages of the disease that can lead to disability [2]. Depending on the patient, the disease may involve episodes of muscle weakness, visual disturbances, balance problems or even difficulties with cognitive function[3]. These symptoms may occur suddenly or gradually increase[14]. It is worth remembering that the first symptoms of multiple sclerosis are sometimes not obvious[15].
How do doctors diagnose multiple sclerosis?
Diagnosing multiple sclerosis is a process that requires accuracy, as the symptoms of this disease can be subtle and easy to miss at first. Moreover, they can resemble other conditions, making it necessary for the neurologist to put the various pieces of the puzzle together to arrive at an accurate diagnosis. The medical history plays an important role - the doctor asks about the nature of the symptoms, their frequency and moments of severity [4,5].
An important tool in diagnosis is MRI. This test allows imaging of brain changes that are characteristic of MS. Sometimes additional investigations such as lumbar puncture are performed. [6,7].
Highly effective therapy - HETA
Multiple sclerosis has undergone a huge shift in treatment with the introduction of high-efficacy therapies, known as HETAs (Highly Efficacy Treatment Agents). In the past, a diagnosis of MS was often associated with a vision of gradual loss of function. Today, with HETA therapies, it is possible to effectively stop disease activity at an early stage, which can allow patients to remain fully active for many years [8].
"Multiple sclerosis is a chronic disease, but we are able to treat it (...) the patient can lead the kind of life they have led before. Our patients at the moment have access to very good therapies"- says Dr Elżbieta Jasińska, MD. The most important thing is to act quickly and effectively. "What science brings us is the information that highly effective drugs can and even should be used at the very beginning - right after diagnosis. This is because inflammatory processes dominate at the beginning. At this stage of our knowledge, we have drugs whose main mechanism is anti-inflammatory. So we aim to stop the inflammatory process. On the other hand, if the patient progresses to the stage of neurodegenerative changes, then unfortunately our options are limited," the interviewee points out.
HETA as first-line therapy
From the end of 2023, Polish patients with multiple sclerosis can benefit from a breakthrough change in treatment - highly effective therapies are available at an early stage of the disease, as part of first-line treatment. This is a huge step forward that allows doctors to apply the most advanced therapies as soon as the diagnosis is made, making it possible to stop the progression of the disease before it causes irreversible changes in the body [9,10,11].
The possibility of implementing HETA at an early stage of the disease is in line with international standards developed by the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS) and the European Academy of Neurology (EAN). This position is also supported by Polish experts, who point out that treatment with highly effective drugs as first-line therapy is not only an opportunity for better therapeutic outcomes, but also a response to patients' needs [12, 13].
Personalisation of treatment - a decision made together with the patient
A personalised approach is fundamental in the treatment of MS - it is not only the choice of drug, but also the adaptation of therapy to the patient's lifestyle and plans[16]. As Dr Elżbieta Jasińska emphasises, the personalisation of treatment is based on a frank conversation during which the doctor and patient decide together on the best course of therapy.
The patient should feel that they have a say in what happens to their health, Dr Jasinska points out. This is particularly important in situations that require a special approach, such as women planning a pregnancy, 'When we make a diagnosis of multiple sclerosis and a young woman sits in front of me we have to take all her life plans, needs, education, profession into account when choosing a therapy. We do this together. My role is to present to the patient what the options are, how the different groups of drugs work and what goals we can achieve with them (...) Moreover, the expert adds that multiple sclerosis does not exclude breastfeeding "we have drugs that are completely safe for our breastfeeding mothers," concludes Dr Jasinska.
The final choice of therapy, however, is more than just a medical issue. It is also about trust, which is built through open conversation. As Dr Jasinska notes, when a patient understands their disease and feels they have a say in their treatment, they are more likely to comply with recommendations, which translates into better outcomes and greater psychological comfort.
Curious about the topic? Go to: www.zapytajosm.pl
The 'Patient First' programme is available on multiple platforms, including Spotify and Google Podcasts.
The episode's partner is Novartis Poland. FA-11352557/I 2025
Transcription
Monika Rachtan
Hi, Monika Rachtan. I would like to welcome you very warmly to the next episode of Patient First. The topic of our conversation today will be multiple sclerosis. That's right. It turns out that the moment the first symptoms appear, it is very important to contact a doctor and start the diagnosis. And why? Because we have a very effective treatment that can actually save the patient from disability. And it is this treatment landscape that I will be talking about today with my guest, and that is Dr Elżbieta Jasińska. A very warm welcome to you. Good morning, doctor. Well, what are the symptoms in us healthy people who feel well every day? We are active, we go to work, we take care of our children should worry. When it comes to the first symptoms of sclerosis.
Elżbieta Jasińska
We should not underestimate any symptoms that will be new to us, especially in the context of multiple sclerosis treatment or diagnosis. What is important are symptoms that appear either very suddenly are significantly exacerbated, or are of such a gradual build-up, but are very persistent for us.
Monika Rachtan
Well, but multiple sclerosis particularly affects young people, those in between. These first symptoms appear between the ages of 20, 25, 30, but they can also appear earlier. And absolutely these healthy people do not think that such a severe and serious disease could happen to them. So what do you need to look out for? Is it the headache or the hand tremor? What are the key symptoms of scleroderma?
Elżbieta Jasińska
The key ones are focal symptoms, which are associated with the formation of inflammatory lesions in the brain, followed by melanin damage as a result of this inflammatory process. It takes us about 10 such foci to statistically develop clinical symptoms. And these motor symptoms, i.e. paresis, balance disorders, dizziness, are the symptoms that most often force patients to see a doctor. However, one of the first symptoms that go unnoticed, which annoy patients, may not affect their quality of physical activity, but their quality of life. Certainly it's sensory disturbances and it's sensory disturbances in over 30% patients that are the very first symptoms that a patient will experience. And these are the young women, who are in their 20s and 40s, who experience numbness, tingling of various kinds of discomfort, sometimes of a burning, burning nature. They report it to the doctor. And unfortunately this is not a symptom specific to multiple sclerosis. Therefore, it is difficult to match it to this multiple sclerosis and we often then look for other causes, such as vitamin deficiencies, electrolyte disorders.
Elżbieta Jasińska
Sometimes we combine this with anaemia. These first symptoms in our patients are of a withdrawing nature. This is the case for the majority of our patients, so they are often missed, overlooked, often forgotten, sometimes actually recorded in the medical records, while sometimes even forgotten by our patients.
Monika Rachtan
Doctor, what does it look like in terms of statistics? Do you happen to make a diagnosis at this early stage, when sometimes these very symptoms that you were talking about occur. But is there a chance that such a patient is seen by a neurologist? He or she goes through the diagnostic pathway and has a diagnosis made? I see hope in primary care physicians, however, who catch these symptoms and refer them to a specialist.
Elżbieta Jasińska
Yes, if these symptoms are bothersome enough for the patient to report to their GP, the doctor will be alert and refer to a specialist. It is then easier for us to assess the severity of these complaints and guide further diagnosis. We must remember that the diagnosis of multiple sclerosis is not an easy process. It can be compared to putting together a jigsaw puzzle, so each piece must fit together. It is not an intuitive diagnosis and we do not make it just because a patient has symptoms. We need to support this diagnosis by performing additional tests.
Monika Rachtan
What kind of research is this?
Elżbieta Jasińska
The main one is MRI. At the moment, it is the primary examination in neurology. Ideally and preferably, we would like to be able to perform an examination not only of the head alone, but also of the cervical cord. It would be good if this diagnosis could also be supplemented with an MRI of the thoracic spinal cord. These are the basic principles of diagnosis. Plus, of course, clinical signs, i.e. at least two casts. If we have two casts in our patient typical of different foci, that is, they will correspond, there will be differences in these symptoms between them. Then we can say with a high degree of probability that our patient has multiple sclerosis. Of course, this diagnosis is made under conditions, usually in a hospital setting, because we also need a very specific test for multiple sclerosis. This is an examination of the cerebrospinal fluid and the finding of oligoclonal striations in the cerebrospinal fluid, which are special, special proteins. It allows us to reinforce this diagnosis.
Monika Rachtan
Well, exactly, and when does the patient have a diagnosis? Patient. Patient. Because we also didn't mention that women get multiple sclerosis much more often than men. What are the statistics here?
Elżbieta Jasińska
Women are 2 to 3 times more likely to be affected than men. This statistic, If we talk about the projected remission form, this statistic evens out somewhat. That is, roughly one man to one woman, if we are talking about the primary progressive form. The difference between these forms is, of course, that in the primary progressive form, patients experience relapses, followed by improvement, relapses, i.e. the appearance of new symptoms or an exacerbation of those that the patient had previously experienced. In contrast, patients with the progressive form, with the primary progressive form, do not experience these flares, while they may experience minor exacerbations in the course. The characteristic feature here is a gradual build-up of disability and this is the form that more often affects people over 40 years of age. And sometimes there is this slight male predominance.
Monika Rachtan
And now we have just made the diagnosis. The patient finds out they have MS And what happens next? Because this is the kind of information that affects your whole life. She says stop for a moment, now everything is going to change. At least we imagine it that way. This sclerosis, because for many years in Poland it was associated with Disability. With isolation. With not being able to work or actually having to change your whole life? What does it look like today?
Elżbieta Jasińska
Today it looks very different. I think a patient shouldn't look at a person who is experiencing the first symptoms of multiple sclerosis. Shouldn't he look at the disease as something that is the only part of his life? Of course it will affect his life, it will require him to change some of his life goals. But what he has worked out so far, how his life has gone, does not change. His goals can still be pursued. This is not a diagnosis at the moment of multiple sclerosis. It is a diagnosis of a chronic disease, still serious and incurable, of course, but a disease that we are treating, for which we have the tools, where we are able to slow down these inflammatory processes, slow down the progression of disability, reduce the number of throws. Therefore, we are reducing this stress. Whereas what you said, or asked me. Diagnosis and what happens next? What happens to the patient? Well, unfortunately, our patients experience a very high level of anxiety. It is fear. It is a new situation for our patient. At times, aggression is also clearly felt in the office. Clearly these negative emotions, this anger prevails.
Elżbieta Jasińska
And here it is the role of the doctor and psychologists to support the patient on this path, to introduce him to the current state of knowledge and to the possibilities available to us.
Monika Rachtan
When we talk about collaboration with the GP, collaboration with the gynaecologist and pregnancy planning comes up. Well, in the case of these highly effective therapies, can we also enter into this pregnancy planning process here with the patient if she is taking the therapy? What does this look like? How do you organise this?
Elżbieta Jasińska
If we prepare patients for pregnancy, if the patient expresses a desire to have offspring, because we also have to remember that not every young woman, despite her young age, being between 20 and 40, that is in this productive period, will want to have offspring. Clearly. And here we are not dismissing the role of the gynaecologist either. Here, women, women should simply have a gynaecological examination. On the other hand, coming back to the problem of pregnancy or, let's say, not so much the problem as the subject of pregnancy, patients usually prepare themselves sensibly for this process. They ask the question. In fact, I try, as we said at the beginning, to talk about it the moment we start therapy. What drug do we choose? Is the patient going to be planning an extended family?
Monika Rachtan
So does it matter to already know at the beginning? To answer that question. Doctor, but just, And if she says yes and says today is the day I start planning my family and trying for a baby. So what happens then? Does the treatment change? Are these high affective therapies discontinued or what does it look like?
Elżbieta Jasińska
Well, it is individual. But if the patient says now, we need to analyse her MRI result, to know, to ask her. I think that if we are managing a patient, then let's say we know how many casts the patient has had in the preceding for this visit to us. In the surgery. Well, assuming this is the first visit, well, at least the patient has had one flare-up in 12 months, so we don't wait. We ask the patient that if we want to prepare well for this, then of course a conversation with the gynaecologist, so that after, say, a year, when we no longer see features of activity in the MRI, when there is no projection activity for a year of therapy. So that the patient is not surprised by, let's say, some gynaecological problems that will prevent her from getting pregnant. So this is such a preparation stage. Of course, we also encourage her to take vitamin D3, to take folic acid. However, the most important thing is that we include a highly effective therapy, because we don't have much time if she wants to get pregnant quickly. Well, then we have a short time to stop the disease as quickly as possible, as intensively as possible, and to stop the disease effectively.
Elżbieta Jasińska
So if over the course of a year, well, ideally we encourage these patients, it all depends. It's a very individual process, very individual decisions. If it's a young girl, we can determine that if it can be determined. Of course we know that a lot of pregnancies are unplanned pregnancies. There are pregnancies despite effective contraception. On the other hand, if we have this ideal period, in my opinion, it is such a period of at least one year. We can stretch it out to two years and then, depending on what ineffective therapy we have, we can either discontinue the medication or stop it in accordance with the current provisions in the summary of product characteristics. Well, unfortunately, we have to discontinue these medicines, even though medical knowledge allows us to continue some of them, some of them.
Monika Rachtan
So they are safe even for a pregnant woman. And are they safe for a breastfeeding mother? Can women who have been treated with high affective therapy before becoming pregnant then breastfeed the baby? Or do the drugs already come back at the stage when the baby arrives and continue during breastfeeding.
Elżbieta Jasińska
We have medicines that are completely safe for our breastfeeding mothers. We also have medicines that we can include. It depends on the size of the molecule. We can include just after that first period when the milk changes its consistency from colostrum, when the nipple is more permeable to large particles. If this stage passes, finishes, then we can safely give drugs even to breastfeeding mothers. This is all we have to take into account here. This balance between gain and loss. Usually, if we have protected the patient well from becoming pregnant, if this cooperation between us has gone well, that is, two years the patient has not experienced a flare, there have been no changes in the MRI. she has passed the pregnancy without complications. We have the patient safe enough that we can still refrain from starting therapy again. Ideally, on the other hand. I think it's also very individual, because some patients are simply afraid of a flare-up right after the solution. And we also see this in studies of the untreated population. On the other hand, the situation is completely different in the case of patients who have started therapy and it was planned.
Monika Rachtan
Planned and thought through. It's very important how your doctor looks at how it used to be and how it is today, because you're a doctor with many years of experience And I, 10 years ago, when I heard the word multiple sclerosis, I thought the poor girl will definitely never have children again. Definitely never again. I once interviewed a canoeist who had just been diagnosed with multiple sclerosis and she told me at the time that her life was coming to an end, although 10 years ago some therapies were already available. On the other hand, just when she is looking from the perspective of an experienced professional, what would she like to say to people who have heard a diagnosis of multiple sclerosis.
Elżbieta Jasińska
That it is a chronic disease, but we are able to treat it, we are able to reduce the build-up of this disability, stop the appearance of new foci, stop the appearance of episodes. The patient is able to lead the kind of life they have led before. Our patients at the moment have access to very good therapies, very good, without these side effects. What I've seen, going back to this past of ours, what was it like in the past? Our patients were experiencing flare-ups, our patients were experiencing side effects associated with the therapies we have. There were voices like this. Patients complained that the disease wasn't as burdensome as the treatment was. Now this has changed completely. We have medicines that. Patients highly effective, highly effective, which patients can use at home, which we can give intravenously once every six months, which we can select, individualise this therapy according to our patient's needs.
Monika Rachtan
The neurology specialty is one where these difficult diagnoses, which have a real impact on the health and life of patients, are said often. And now from the perspective of a doctor, a specialist, but also a woman, how does your doctor approach this, that already today, when I give information about MS, well it's not in the back of your mind that it's this disability, that it's all these problems that the patient may or may not be thinking about, It's just that immediately your doctor pulls out such a retinue of different modern therapies and actually starts to tailor-make a therapy to suit the patient's needs. Because it's not just your doctor's personal choice which therapy the patient gets, but many things are taken into account here. How old is the patient, what kind of plans does she have, what kind of parenting plans does she have, is she a young woman who already has children, or is she going to try to have a child after all? Well, how does your doctor look at this moment from the perspective of a woman and a specialist?
Elżbieta Jasińska
This is a difficult moment for us, for our patients. On the other hand, when we make a diagnosis of multiple sclerosis and there's a young woman sitting in front of me, we have to take all these life plans of hers, these needs of hers, her education, her occupation into account when choosing a therapy. And we do this together, we determine of course. My role is to present to the patient what the options are, how the different drug groups work and what goals we can achieve with them. And if the patient is a young person, that is the most important goal for the doctor. My goal is to stop the inflammatory activity of the disease immediately, as soon as possible. And we have such data that our patients who maintain effective treatment for one year, ideally two years, the moment they become pregnant and the pregnancy can, it will be maintained. With each week, the risk of a flare in such a patient decreases so that in the third trimester it is already the lowest. Unfortunately, it increases just after termination and hence these discussions of ours about which drug to choose. They must also be based on the patient's life plans. That is, which of these drugs will not only be the most comfortable for her, but also the safest and which we can return to very quickly after delivery.
Monika Rachtan
It is this choice, this treatment, this treatment that is for the patient, for the patient, it is their treatment and it is supposed to be appropriate to their needs. And now the question is, if you are making a decision, looking at all the factors you have mentioned, does this question arise for the patient: what do you think? Which treatment would you use for yourself, not looking at things related to medical knowledge, but just this convenience, plans? Is this conversation, the patient the doctor having?
Elżbieta Jasińska
Yes, yes, it happens regularly. Patients react in different ways. Sometimes I hear that I am the electrician or I am the accountant. If a doctor asks me how to settle the bills, I am happy to help. Not, however, with the choice of therapy. However, I think that the development of knowledge, access to this information, what you are also doing, enables our patients to broaden their horizons, broaden their knowledge and they are more aware of what questions to ask at the doctor's surgery, what medicine would be good for them. It is not always this decision, this choice that is right, because sometimes patients rely not only on internet information, but also from their neighbours. They ask patients who have never been treated, for example, or who have experienced those previous therapies that were nevertheless at high risk of side effects. Where they occurred. Pseudo-flu-like symptoms. Where depression was present. Where patients were dropping out of therapy during treatment due to side effects, with little or no regard for the fact that their physical condition might worsen.
Monika Rachtan
It has been said here today that you have in your possession highly effective therapies. Exactly what does such treatment consist of? When is it introduced, at what stage? Are we already talking here about patients with more advanced disease, or can such high-affective therapy also be introduced as soon as the diagnosis is made?
Elżbieta Jasińska
Until last year, we had a division of drugs into first-line and second-line, so unfortunately we could not decide on highly effective drugs for all patients. What science brings us, on the other hand, is the information that highly effective drugs can and even should be used right at the beginning, right after diagnosis. This is because at the beginning, as I said, inflammatory processes dominate, and at this stage of our knowledge we have drugs whose main mechanism is anti-inflammatory, so we aim to stop the inflammatory process. On the other hand, if a patient goes through this stage of neurodegenerative changes, is that the dominant process in the primary progressive form? Then, unfortunately, our options are limited, so we act quickly in order to react quickly and stop the progression of the disease right from the start, giving the patient a sense of security. Because if there are no relapses during the first year or two, we have no new lesions. Patients are very vigilant in checking their MRI results. Then they have a sense of security, they know they are being treated and then their life takes a back seat, it gains momentum.
Elżbieta Jasińska
I think these first two years are crucial.
Monika Rachtan
Exactly, because it is very important to send such a signal to the patient that I am a doctor you can trust, that today he has modern therapies which can make a real difference to your health situation. And if, in these first two years, it seems to me, the patient gets this signal that actually this doctor knows what he is doing, these therapies are helping me, then this effectiveness of treatment on the part of the patient and this compliance is much better, because I know that a few years ago there were situations where patients, because the treatment was ineffective, refused therapy or stopped contacting the doctor for a few years and came back with a much greater disability, because they were no longer able to function. And today, when there are these highly effective therapies, this probably doesn't happen.
Elżbieta Jasińska
Yes in the practice. What is most important in the practice is indeed trust, but also the sincerity of our patients. Is the patient really tolerating the medicine well, is he or she accepting this treatment? Hiding from us, from me, whether the patient has taken the medication or not, is acting to the detriment of our patient, to their own detriment, to their own detriment, to their own deterioration. On the other hand, it is always office visits and these conversations are very difficult. On the other hand, indeed the introduction of highly effective therapies has also enabled us to have greater control over the administration of compliance, i.e. this compliance of treatment is much higher.
Monika Rachtan
And now what does this monitoring of the patient look like? Because the patient is given the drug, in fact they completely have to rely on the doctor for that first administration, well because I hear that it is a highly effective therapy, that probably everything will be fine and there will be no further symptoms that will lead to disability. But then you have to verify that what you have done is working and what this monitoring of the patient looks like. In addition to this phone call that takes place does the patient feel well?
Elżbieta Jasińska
Yes, we regularly check blood tests, basic blood tests, because there is no need for any detailed monitoring of the patient here, but we pay attention to whether infections are more frequent, whether the patient reports any side effects. Minor side effects do occur after the first injection and we warn the patient about this too. Subsequent infections. Generally, most of our patients are asymptomatic. 80% of our patients really tolerate the treatment perfectly. We check. In addition to that, once a year we do an MRI scan and we check the features of activity of this radiology, that is, whether a new lesion has appeared, whether the lesions are active, that is, enhancing After the administration of contrast, we do a neurological examination, a full neurological examination. We assess precisely this disability of our patients. A special EDS scale is used for this. We also assess the cognitive function of our patients, we carry out a depression scale. This is all at this annual visit, because this is the evaluation of the assessment.
Monika Rachtan
The balance, such.
Elżbieta Jasińska
We do the balance sheet like this. We do this evaluation once a year. However, depending on the needs, sometimes we have patients who do not go on therapy so easily, who experience side effects and sometimes some exacerbations of the disease. Then we have to be more vigilant and sometimes this MRI has to be done, for example, after six months.
Monika Rachtan
That is to say, it is very important that the patient cooperates with the doctor, that not only does the doctor himself monitor how this treatment is working, but that the patient is alert to any symptoms that occur, that appear, that are new, and then that he reacts quickly and contacts his doctor. This is the one.
Elżbieta Jasińska
An ideal, ideal situation, whether with a doctor or a nurse. In our case, this is the communication system. Through the nurse also works perfectly. Patients have a lot of trust. To the lady nurses. Some of these questions are about. Purely such technical procedures. Sometimes there is a problem with the administration of a drug, sometimes a bruise will form at the site of administration. The patient gets nervous, they don't know if they've administered correctly, they don't know if it's a worrying signal for them. Worthwhile. It's worth it to sort of inspire that trust, to have that confidence and that good communication between each other. If the patient has this openness, if we are able, if we are available to them, then they should take advantage of it.
Monika Rachtan
And is this treatment that the patient is receiving, are these highly effective therapies in such a form that the patient administers them to himself at home. Does he necessarily have to come to the centre for the administration of the medication?
Elżbieta Jasińska
This varies. There are therapies that the patient actually has to come to our centre for. However, we also have therapies that the patient can use at home. These are different, different, different forms of administration. They are not only injectable therapies, but also oral therapies. They are also getting wider and wider. It is a portfolio of medicines for our patients and getting healthier. Our. Our patients. Our charges.
Monika Rachtan
Doctor, if we have a broad portfolio of drugs, is there a possibility that a patient, for example, no longer wants to take this form of therapy because it doesn't suit them, it doesn't suit the way it's administered, and can they change under the drug programme to another available highly effective drug?
Elżbieta Jasińska
Maybe, Maybe after talking to the doctor. Of course, it is such a joint decision. It is also worth listening to the doctor's opinion as to whether this therapy would be better for me. On the other hand, there is a possibility and sometimes we use this possibility, especially if the patient does not accept the therapy or has changed her lifestyle. Is it precisely this young girl who becomes pregnant? Sometimes we have to change this therapy in the course.
Monika Rachtan
And what are the key benefits of cheat therapy?
Elżbieta Jasińska
The key is precisely to stop inflammatory activity. This is the most crucial element at this point. That is, not only do we reduce this inflammation that we have, but thanks to this, if it happens at an early stage, these abilities of our organism are efficient enough that part of this outbreak will still be repaired. That is why we are keen to start this therapy as early as possible. Of course, another, further goal we are achieving is to reduce the number of casts. So that's the goal we're still working towards. And here we still have a big, big shortfall. It is, however, slowing down disability. We talked about what it used to look like, what it looks like now. It used to be that we and our patients were focused on reducing the number of casts. The cast was our patient's biggest problem. Back then it caused the most fear, the most anxiety. And how.
Monika Rachtan
Is it now?
Elżbieta Jasińska
It is now that patients don't have as many casts. It's a really clear, clear, clear reduction. So here free our patients from the casts, from the inflammatory activity now expect to slow down the progression, the disability.
Monika Rachtan
And this is being achieved.
Elżbieta Jasińska
We are trying. This is the quiet progression. It is still there for us, it is still out of reach as we would like it to be, that one day our patient will obtain.
Monika Rachtan
And when it comes to the doctors themselves, what is it for you as a doctor that is such a factor that turns on that light in your head that maybe it would be worthwhile to look for a different treatment for the patient, a different therapy, that you just reach for one drug and not the one that has been used so far. What is the factor that most catches your doctor's eye?
Elżbieta Jasińska
Well, for me, however, from a physician's point of view, it is the features of disease activity, that is, the appearance of a new outbreak in the second year of therapy, for example, or the appearance of active outbreaks. This is kind of a primary goal. Of course, the occurrence of some flare-ups, sometimes mental deterioration is not necessarily a physically, let's say, tangible flare-up. However, a very, very important aspect is also the quality of life of our patients. And it happens that we change therapy because of the occurrence of side effects, because of intolerance to a drug, because of the occurrence of symptoms such as burning skin or redness for a young girl, for example. For a young woman, this is a big problem. One of my students was asked out of class because her skin suddenly turned red and the lecturer was frightened that she had and asked the patient that something bad was happening. During this class he asked the patient to see a doctor. Also, it is sometimes these side effects of medication that can be distressing for our patients.
Monika Rachtan
And what is the role of the primary care physician when it comes to collaboration between the neurologist? The patient in this whole process of multiple sclerosis care, Because when it comes to oncology patients, for example, it is often the case that if a patient is being treated for a disease, the primary care physician. So a little bit prefers not to move this patient, in order not to harm him. And when it comes to multiple sclerosis, are there also elements of the patient's life that may affect the primary care physician and may here require your cooperation, your getting along, so to speak, so that this patient is best managed, e.g. If the patient has the flu, has COVID, these things also happen.
Elżbieta Jasińska
Of course, these are urinary tract infections, these are respiratory tract infections. Our patients also experience such infections. This is also due to the fact that we are running a therapy that modifies the immune system, so we can expect slightly more frequent infections in our patients. This is also due to the course of the disease itself. One of the additional symptoms of multiple sclerosis is sphincter disorders. This is an issue of neurogenic bladder, for example, this is an issue of urinary retention. And therefore increased. Increased risk of infection. And in such cases, this cooperation really works out very well for us. However, here it is a question of choosing the right treatment. And this is where colleagues sometimes call and ask if they can. We issue certificates, explain to patients which drugs they can take. We write it down on cards, we issue information that the patient may or may not use such drugs. Usually, such a request is made, and this is also where the nurses play a big role. They take a really active part in this. They redirect. They are also able to sort of highlight, select the patient who, however, for whom communication with a neurologist is necessary.
Elżbieta Jasińska
Also such discussions as the topic of vaccination, for example. Well, just about.
Monika Rachtan
This is what I wanted to ask. Can patients with MS be vaccinated?
Elżbieta Jasińska
They can. just in terms of preventing these viral infections or bacterial infections. We encourage our patients to have vaccinations. The most common vaccination at the moment is the one related to whooping cough. We are aware of the increase in whooping cough cases. Our patients are also concerned about this, asking questions, enquiring.
Monika Rachtan
Let us also remember that every adult Pole should. every 10 years. Every adult should be vaccinated when it comes to whooping cough. This is very important, and it is still something that does not resonate when it comes to this very vaccination.
Elżbieta Jasińska
Pertussis just happens to be vaccinated along with diphtheria and tetanus. Again, these are indeed vaccinations that we should repeat, but we also have vaccinations against human papillomavirus. Here, too, we encourage our patients to be vaccinated against influenza. And finally, the very important pneumococcal vaccination. And we do see a marked reduction in the risk of infection in our patients. There are also times when I make use of GPs. This was the case last week, when one of my patients had just decided to get vaccinated against pneumococcus, but came in for an appointment with a cold. And this is where we need a little bit of support from the internist or GP. Can such a patient with these symptoms be vaccinated?
Monika Rachtan
Doctor, how do you look at this? The drug programme has changed. It will probably still change a lot. As more modern therapies come in. On the other hand, I wonder if you have any history of having met a patient early on when she was diagnosed and just reached for this high affective therapy and got such results that you say Oh, this is the patient I want to talk about, because I didn't expect it to go so well.
Elżbieta Jasińska
Yes, we have a lot of such patients. Working with patients since the Platform drugs. However, the introduction of highly effective therapies is a great pleasure. We see patients who experience no side effects, patients who are happy with their lives, no casts, no changes in this MRI I keep coming back to this because I am a doctor and this is our tool. And there are more and more of these patients, and as a result the visits are less mentally taxing. We are not looking at it. The increase in disability, for those patients who just a few years ago were coming in a wheelchair and expecting to be helped. At the moment, our patients are stable for many years.
Monika Rachtan
It is the highly affective therapies that have completely changed the landscape of multiple sclerosis treatment. We are no longer talking about disability, we are no longer talking about a life of pain and suffering, and we can talk about being active people who can fulfil their dreams, who can be parents. Dear ones, if you are in such a situation that you have been diagnosed with multiple sclerosis, it is imperative that you invest in this conversation with your doctor and ask about non-effective therapy, so that you are already at the very beginning, get this most effective treatment that will save you from disability. Doctor, thank you very much for our conversation today. Thank you very much for accepting the invitation to join my programme.
Elżbieta Jasińska
Thank you.
Monika Rachtan
My guest was Dr Elżbieta Jasińska, a neurologist, and this was the programme Patient First. I thank you very much for your attention. I invite you to subscribe to our social media channels. If you are looking for more valuable content, subscribe to us on YouTube and Spotify. Monika Rachtan. You are very welcome!
Previous episodes

An app that will take care of your family when you are gone. Episode 89
Have you ever thought about what will happen to your affairs, documents and loved ones when you are gone?

Coalition for the Premature - 12 years of fighting for the health of the little ones. Episode 87
What is life like for families of premature babies and what support can they receive?

Obesity in Poland: How to stop the growing problem? Episode 86
Did you know that obesity already affects 57% Poles, and its complications can shorten life by up to a dozen years?

The digital challenges of modern parenting. Episode 85
According to research, as many as 83% Polish children aged 7-14 have their own mobile phone.